Day-case Haemorrhoidectomy
What are Haemorrhoids?
Haemorrhoids are swollen or inflamed vascular structures located around the anus or in the rectum. They are classified into two main types: internal and external haemorrhoids.
Internal Haemorrhoids occur within the rectum and usually do not cause significant pain, although symptoms like bleeding or leakage may occur. Common causes include chronic constipation, increased abdominal pressure, and pregnancy.
External Haemorrhoids develop around the anus and can form a small lump, often leading to severe pain and discomfort. These are typically caused by prolonged straining during bowel movements, trauma to the anal area, or poor blood circulation.
Symptoms of Haemorrhoids
-
Pain: Internal haemorrhoids are generally painless, while external haemorrhoids may cause severe pain, especially during bowel movements or prolonged sitting, walking, or standing.
-
Bleeding: Visible bleeding can occur during bowel movements or when straining, typically bright red and noticeable on toilet paper or in the toilet bowl.
-
Itching and Burning: Patients may experience itching, burning, or a prickling sensation around the anus, which can worsen with prolonged sitting or friction.
-
Lump: External haemorrhoids often present as a small lump that can be felt around the anus, which may be soft or hard and cause discomfort.
-
Discomfort: A sensation of pressure or discomfort in the anal region may be felt, akin to the presence of a foreign body.
Risk Factors for Haemorrhoids
-
Age: Aging increases the risk of haemorrhoids, as connective tissues weaken and blood vessels become more prone to dilation.
-
Chronic Constipation: Prolonged constipation or excessive straining during bowel movements elevates pressure in the anal area, leading to haemorrhoid formation.
-
Excessive Straining: Straining during bowel movements heightens pressure in the anal region, increasing the likelihood of developing haemorrhoids.
-
Genetic Factors: A familial predisposition to haemorrhoids may indicate a higher risk.
-
Pregnancy: The expanding uterus can exert pressure on abdominal and pelvic blood vessels, leading to haemorrhoid development.
-
Prolonged Sitting or Standing: Extended periods in one position can hinder blood circulation, causing blood to pool in the anal region.
-
Obesity: Increased abdominal pressure associated with obesity can contribute to haemorrhoid occurrence.
-
Poor Diet: A low-fiber diet, dehydration, and high-fat intake can lead to constipation and the development of haemorrhoids.
Who Needs to Undergo Haemorrhoid Surgery?
Surgery may be necessary for treating haemorrhoids in the following situations:
- Severe Symptoms: If symptoms are severe and do not respond to conservative treatments, such as intense pain or significant bleeding.
- Thrombosis: Thrombosed external haemorrhoids can form hard lumps causing severe pain, necessitating surgical intervention if conservative measures fail.
- Internal Haemorrhoid Prolapse: Prolapsed internal haemorrhoids that cannot be repositioned may require surgery.
Chronic Haemorrhoids: Patients with recurrent and difficult-to-treat haemorrhoids may benefit from surgical options.
The decision to proceed with surgery should be based on the severity of symptoms and the effectiveness of conservative treatments. Consultation with a qualified medical professional is recommended for diagnosis and treatment options.
Overview of Haemorrhoid Surgery
Traditional Haemorrhoidectomy (Open Haemorrhoidectomy): 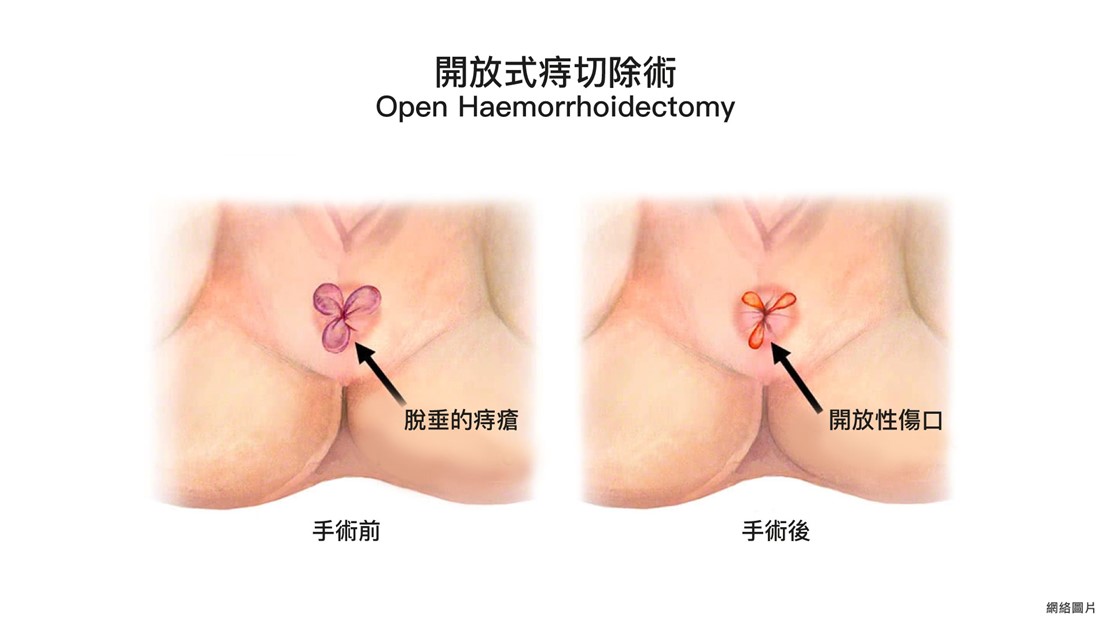
This method is suitable for severe haemorrhoids, allowing for the removal of both internal and external haemorrhoids. Techniques may include radiofrequency, cautery, or traditional surgical instruments. The procedure takes about 30 to 45 minutes and generally involves more trauma.
Stapled Haemorrhoidectomy (Stapled Haemorrhoidopexy):
This commonly used technique employs a stapling device to reposition prolapsed tissue back into the anal canal and excise the mucosa of internal haemorrhoids. It reduces blood supply, allowing the haemorrhoids to shrink postoperatively. Compared to traditional methods, it results in minimal external wounds, less pain, and shorter recovery times.
technique employs a stapling device to reposition prolapsed tissue back into the anal canal and excise the mucosa of internal haemorrhoids. It reduces blood supply, allowing the haemorrhoids to shrink postoperatively. Compared to traditional methods, it results in minimal external wounds, less pain, and shorter recovery times.
Note: Patients with severe external haemorrhoids, mixed internal and external haemorrhoids, or anal stenosis are not suitable candidates for circular haemorrhoidectomy.
Comparison of Two Types of Haemorrhoidectomy
|
Feature |
1. Traditional Haemorrhoidectomy |
2. Stapled Haemorrhoidectomy |
|
Procedure Description |
Involves excision using an electrosurgical knife, with closure via sutures or left open.
|
Utilizes a stapling device for excision and repositioning.
|
|
Postoperative Pain Level
|
Generally associated with significant pain.
|
Typically results in less pain.
|
|
Wound Care
|
Requires disinfection after each bowel movement.
|
Minimal care needed if no external wound. |
|
Recovery Time
|
Longer |
Shorter |
|
One-Year Recurrence Rate
|
1% |
8% |
|
Cost
|
Generally lower cost. |
Higher cost due to equipment.
|
Doppler Haemorrhoidal Artery Ligation, HAL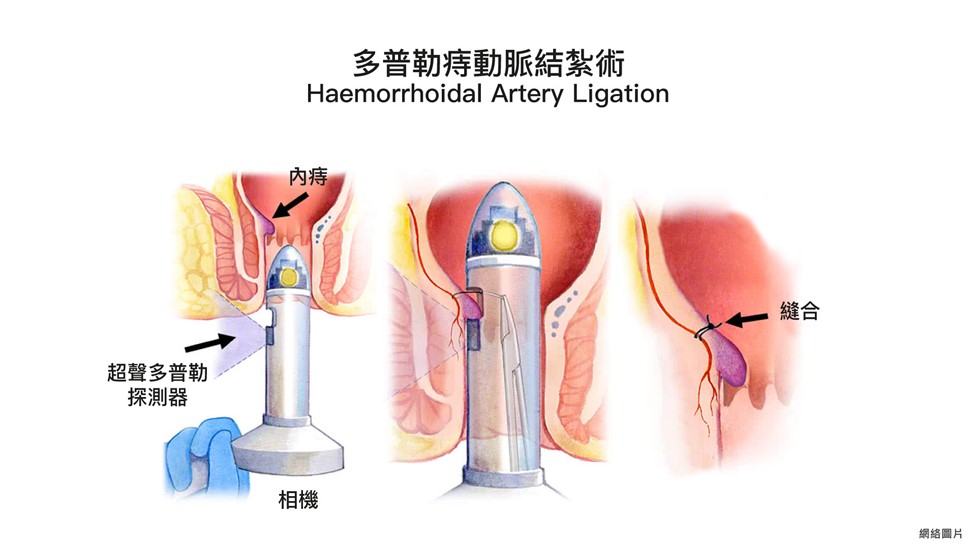 :
:
HAL is a minimally invasive procedure that uses ultrasound to accurately locate haemorrhoidal blood vessels, ligating them to interrupt blood supply and promote shrinkage of the haemorrhoids. This technique is suitable for patients with significant bleeding but no severe external haemorrhoids. HAL is scalpel-free, results in mild postoperative discomfort, and has a low risk of complications, often eliminating the need for hospitalization.
Treatment approaches for haemorrhoids vary based on severity, and physicians may recommend multiple surgical options. If you suspect you have haemorrhoids, consult a physician for an appropriate treatment plan.
Preparation for Surgery
-
Fasting Instructions: Patients are usually required to fast for 6 hours before surgery, allowing only a small amount of plain water up to 2 hours prior to the procedure.
-
Preoperative Medications: Follow prescribed medication instructions, and inform your doctor of any blood-thinning medications, such as Aspirin or Warfarin, as well as herbal supplements.
-
Informed Consent: The doctor will explain the procedure, its rationale, and potential complications. Patients should review this information before signing a consent form.
Wound Care Post-Surgery
-
After surgery, minor bleeding or increased bowel movement frequency may occur for up to two weeks.
-
Gently rinse the wound with a handheld shower after each bowel movement to keep it clean.
-
If a circular haemorrhoidectomy was performed without external wounds, no special care is needed.
-
Patients can shower as usual the day after surgery, avoiding excessive soap or bath oils to prevent irritation.
Follow-up and Recovery
-
Minor oozing and increased sensitivity are common in the two weeks following surgery.
-
Maintain cleanliness of the wound to prevent infection.
-
Dietary adjustments may be recommended to avoid constipation, including increasing fiber intake and hydration.
-
Follow healthcare provider instructions for wound care.
-
Symptoms such as headaches, dizziness, or inflammation should naturally subside within a few days. Pain relief medication may be taken as needed, and patients should ensure adequate rest.
-
Avoid eating until the effects of anesthesia and sedatives have worn off to prevent choking.
-
On the day of the procedure, avoid alcohol, operating heavy machinery, or driving to prevent accidents. Refrain from signing legal documents for 24 hours post-surgery.
-
Patients may leave the facility once the effects of anesthesia have worn off but must be accompanied by an adult.
-
Contact your doctor immediately if you experience pain, swelling, bleeding, signs of infection, or other unusual symptoms.
References
衞生防護中心. 男性常見疾病 - 痔瘡. Available at https://www.chp.gov.hk/tc/static/80041.html
National Health Service. Piles (haemorrhoids). nhs.uk. Available at https://www.nhs.uk/conditions/piles-haemorrhoids/
衛生防護中心. 痔瘡發作 - 並不是一件開玩笑的事. 非傳染病直擊, 第四卷. Available at https://www.chp.gov.hk/files/pdf/ncd_watch_jan_2011_chi.pdf

 3405 8288
3405 8288