Day-case Colonoscopy
Why do you need to get a colonoscopy?
Colorectal cancer, which encompasses both colon cancer and rectal cancer, is one of the most prevalent malignant tumors worldwide. Within the local context of Hong Kong, the incidence and mortality rates associated with colorectal cancer have been observed to be on a consistent upward trend in recent years. Colorectal cancer as the second most common cancer in Hong Kong and there is a noticeable trend towards a younger patient demographic.
According to The Department of Health (DH), in 2021. There were 5,899 new cases of colorectal cancer, with 3,427 cases among males and 2,472 cases among females in Hong Kong. Colorectal cancer resulted in 2,270 deaths in 2022, accounting for 15.4% of all cancer deaths.
If caught in the early stages while the cancer is still localized, the survival rate of colorectal cancer is 91%. There has been substantial proof around the world that colorectal cancer screening can lower the incidence rate of the disease. In the US, asymptomatic individuals regularly undergo screening for colorectal cancer from the age of 50.
Early-stage colorectal cancer symptoms are not obvious and easy to overlook
The common symptoms of colorectal cancer include changes in bowel habits, rectal bleeding, abdominal bloating, abdominal pain, unintentional weight loss, and anemia. However, it is important to note that the early-stage symptoms of colorectal cancer are often not very apparent. Some patients only seek medical attention when they experience more pronounced discomfort, by which time the disease may have already progressed to a more advanced stage.
Factors that may increase the risk of colorectal cancer
Family history, adenomatous polyps, gut microbiome imbalance tend to increase the risk of getting colon cancer. Not exercising regularly, Obesity, certain lifestyle and diet might be linked with colon cancer and rectal cancer. An increased risk of colon cancer is found in people who eat a lot of red meat and processed meat, people who smoke and drinking too much alcohol.
50 or above should regularly receive Cancer Prevention and Screening
The Hong Kong Cancer Expert Working Group on Cancer Prevention and Screening (CEWG), the leading cancer prevention advisory group under The Department of Health, recommends that all average-risk individuals aged 50-75 years, under consultation with their family doctor, should consider faecal occult blood test annually or bi-annually, a sigmoidoscopy screening every 5 years or a colonoscopy screening every 10 years. However a report from Department of Health showed that only 40% of aged 50-75 have undergone any faecal occult blood test/colonoscopy screening.
Some individuals may have a higher risk for CRC and may consider more regular screenings, such as people who carry associated genetic mutations associated with CRC or people who have first degree relatives that were diagnosed with CRC. Individuals with one or more first-degree relative (parent, siblings) who have been diagnosed with CRC are advised to undergo colonoscopy every 5 years starting at an earlier age.
Colonoscopy is the best prevention for colorectal cancer. However, polyps can grow back after they have been removed once. Regular screening tests, such as a colonoscopy, can find colon polyps and have them removed safely.
Colorectal cancer developing sequence
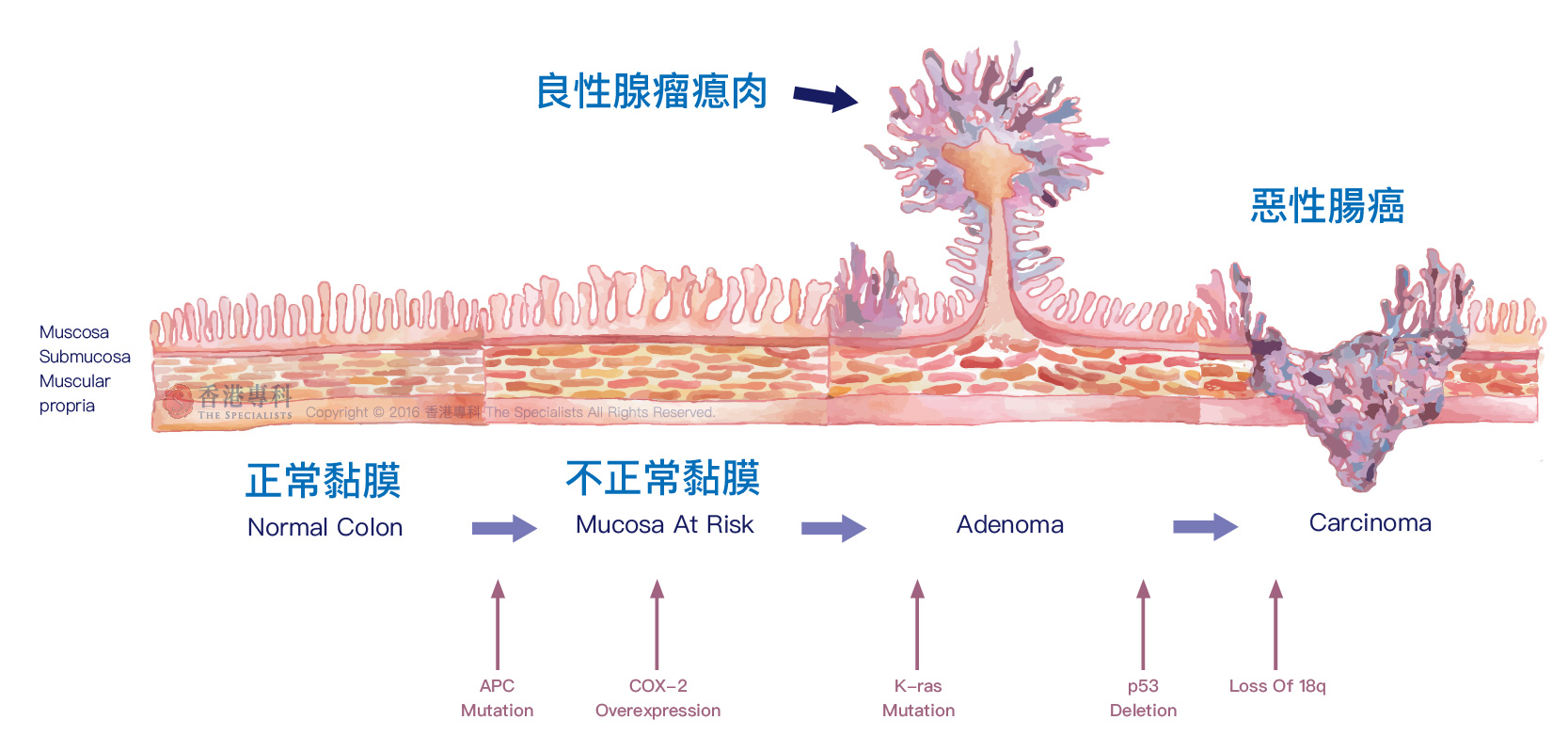
The colorectal adenoma-carcinoma sequence suggests that a clump of cells form the adenomatous polyps that attach to surface of the colon’s mucous membrane, and the adenomatous polyps become cancerous. It takes about 10 years for an adenomatous polyp to turn into cancer. Over 70 percent of colorectal cancers begin as a benign polyp. Removing the polyps can help prevent colorectal cancer from developing. If the polyps are not removed, they could turn into colorectal cancer.
Who should have colonoscopy?
-
Start after the age of 50
-
Have a family history of colon cancer
-
Have per rectal bleeding
-
Experience bloating
-
Change in bowel habits
-
Weight loss
-
Experience unexplained abdominal pain
-
Have suspected colonic polyps
-
Have inflammatory bowel disease
Most colorectal cancers are preventable, hence regular colon screenings are crucial. People aged 50 and above have a higher risk of developing polyps or cancer, a colonoscopy is recommended for this age group even without obvious symptoms. Early detection through screening is key to preventing colorectal cancer.
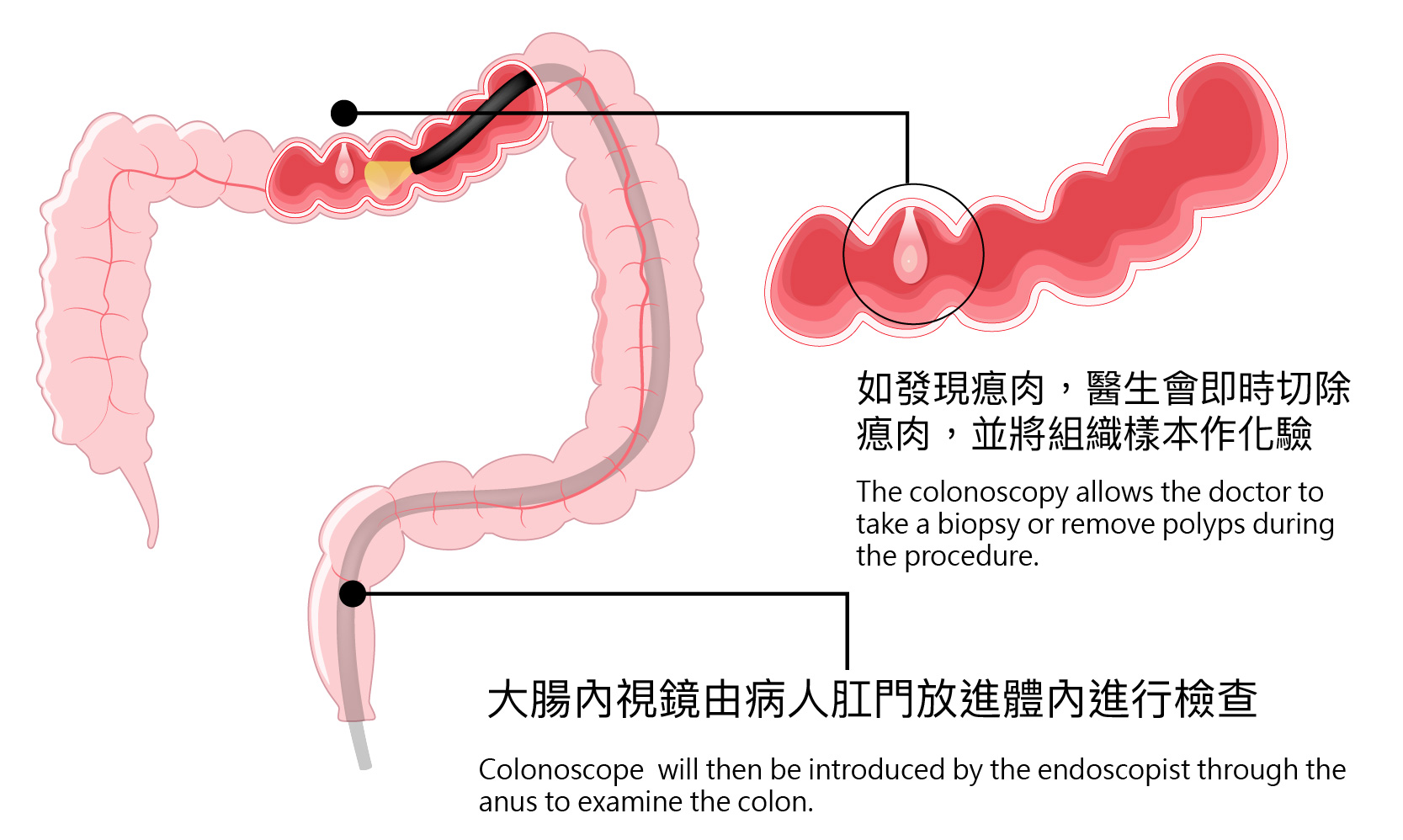
Patients may sleep through a colonoscopy with sedation and will not feel pain. Colonoscopy is the endoscopic examination of the inner lining of the large bowel (colon) with a flexible endoscope. The examination is carried out by passing such a flexible endoscope through the anus to the lower bowel to examine if there is any inflammation, polyp or tumour.
The examination will be performed only when the patient is asleep after monitored anaesthesia care administered by anaesthesiologist, to avoid any discomfort. Anaesthesiologists will participate in providing an anaesthesia opinion prior to the endoscopy. During the procedure, they will constantly monitor the stability of vital signs including pulse, breathing, and blood pressure, making sure vital organs are functioning as normal. Monitored anaesthesia care is a special alternative for patients that require maximum comfort and safety.
During a colonoscopy, the doctor can remove polyps and take biopsies when any suspicious tissues are found. After removal, the biopsy specimen will be sent to the laboratory for testing.
Colonoscopy is a mature technique, and the successful cases and completion rates shown in the data demonstrate that the risks are manageable. You only need to find a reliable medical institution to perform the procedure and fully understand your personal situation and risks with the doctor before the examination. Most colonoscopies can be performed as outpatient procedures in a day medical center, allowing for a safe and quick discharge on the same day.
Learn more about the colonoscopy data from our centre.
How to prepare for the procedure?
Prior to the procedure, patients should:
- A pre-consultation is required during which the doctor is able to determine whether the patient's physical condition is suitable for endoscopy or anaesthesia procedures. And doctor will let the patient know the risks associated with the examination.
- Stop taking iron supplement for 3 days before the procedure. Patients who are taking wafarin and aspirin should inform the doctor in advance. In some cases, doctor may ask the patient to stop taking the medication prior to the examination.
- Stop ingesting high fibre diet/drink including vegetables, fruit, wheat, mushrooms and cereals three (3) days before the procedure. Patients can eat starchy, protein and fatty foods.
- Only intake clear liquid the day before the procedure. Patients can have fish congee and minced meat congee.
- Patients should take the laxative prescribed by the doctor on the day before the test/or in the morning of the test. (Patients are not recommended to buy the laxative by themselves). Before drinking laxatives, patients can prepare 2 litres of electrolyte water, cleansing wipes for skin and petroleum jelly .
- Do not eat anything for 6 hours before the procedure.
- Do not eat and drink anything for 2 hours before the procedure.
- The Doctor will have a brief consultation with the patient to explain the procedure and the risks involved. A consent form will then be signed by the patient.
- Remove dentures, accessories (watches, necklaces, earrings, rings) and metallic objects.
- If the patient suspects that she is pregnant, she should be sure to let the doctor know.
What happens during the colonoscopy?
 |
 |
 |
 |
 |
|
MAC |
The endoscope can be passed into the colon |
If polyps are found, doctor will remove them or take biopsies for analysis |
CO2 will be pumped into the colon during colonoscopy and can reduce abdominal bloating as a result |
The entire procedure should take around 30 minutes |
*The method of anaesthesia is determined by doctor according to the individual patient’s condition.
- To avoid any discomfort, intravenous sedation or anaesthesiologist monitored anaesthesia care will be carried out, and the examination will only be performed when the patient is fully asleep.. Anaesthesiologists will participate in providing anaesthetic opinions to patients prior to the endoscopy. During the procedure, they will constantly monitor the stability of vital signs including pulse, breathing, and blood pressure to ensure the vitality of important organ functions.
- Doctor will apply some lubricant to the anal region. A flexible colonoscope with a diameter of around 1.5cm will then be introduced by the endoscopist through the anus to examine the colon.
- The doctor may take a biopsy or remove polyps during the procedure.
- During the endoscopy process, a small amount of air insufflation is applied to visualize the colon images. It is normal to have cramps and a feeling of wanting to go to the toilet. An alternative gas that can be pumped into the colon during colonoscopy is carbon dioxide (CO2). Unlike air, CO2 is very rapidly reabsorbed into the body from the colon, about 150 times faster than air.
- The procedure will be completed in 30 minutes.
After the procedure
-
After the patient completes the procedure, he/she will be sent to the recovery area. the patient will be cared for and their vital signs closely monitored by dedicated nurses.After the patient wakes up, he/she will be transferred to the private resting room.
-
In the private resting room, in addition to the vital signs monitor connected with the central system, we have an alarm clock, lifesaving alarm, walkie-talkie and other medical equipment. There are also entertainment facilities such as sofas, TV set and magazines. The room is prepared after the procedure to give patient time to wear off the sedation. Family members can accompany during this time.
-
As patient is sedated, he/she should be accompanied by at least a friend or a family member aged above 18.
-
The sedation and the anaesthetics may temporarily affect one's co-ordination and reasoning skills, and patients are advised to avoid driving, drinking alcohol, making any important decisions or signing legal documents within 24 hours after the procedure.
-
Patients can resume their normal diet after colonoscopy. However, if the patient has undergone a polypectomy, he/she will be asked to withhold from consuming certain types of vegetables and fruits within 10 days of the examination.
-
If the patient has undergone polypectomy or extraction of biopsies during the procedure, he/she will be strongly advised to stay in Hong Kong for 10 days after surgery. If the patient cannot promise to stay in Hong Kong for 10 days after surgery, please inform the doctor before the test.
References
Centre for Health Protection. Colorectal Cancer. Available at https://www.chp.gov.hk/en/healthtopics/content/25/51.html
American Cancer Society. Colorectal Cancer. Available at https://www.cancer.org/cancer/types/colon-rectal-cancer.html
Mayo Clinic. Colon cancer. Available at https://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669
Centre for Health Protection. Cancer Expert Working Group on Cancer Prevention and Screening. Available at https://www.chp.gov.hk/files/pdf/cewg_crc_professional_hp.pdf
Kumar et al. (2009). Robbins & Cotran Pathologic Basis of Disease, 8th Edition.
Department of Health. Colorectal Cancer Screening Programme. Available at https://www.colonscreen.gov.hk/en/public/programme/understand_the_suitability_for_receiving_crc_screening.html

 3405 8288
3405 8288