Day-case Gastroscopy
Why do you need to get a gastroscopy?
Stomach cancer as a common cancer in Hong Kong
Stomach cancer which is also called gastric cancer, was the sixth commonest cancer in Hong Kong in 2021. According to the statistics of Centre for Health Protection (CHP), there were 1,306 new cases of stomach cancer in 2021, with 762 cases of males and 552 cases of females, accounted for 3.4% of all new cancer cases. In 2022, it claimed 634 deaths, accounting for 4.3% of all cancer deaths.
Stomach cancer is found high risk among Asian
Asians tend to consume a lot of high-salt, smoked, fried, and grilled foods, together with the habit of dining, which can easily lead to the spread of pathogens. In recent years, patients have also tended to be younger, with records showing the youngest patient being only 30 years old.
Due to modern lifestyle and dietary issues, the stomach can no longer cope. At present, gastroscopy is the most effective detection tool of stomach diseases.
The medical community generally believes that for adults over 40, especially those at high risk of stomach cancer, regular gastroscopy examination is absolutely necessary. After all, early detection and early treatment is the golden rule for cancer treatment.
Patients who diagnosed with Gastric Cancer is more often in young people
- Diet factor
Gastric cancer risk may increase when young people have an unhealthy diet habit and food consumption such as processed, grilled, or barbequed meats.
- Family history
When individuals had a first-degree relative with gastric cancer, their relative risks to develop gastric cancer ranged from 1.5-fold to 3.5-fold in studies. Those young people should be more alert and consult doctor if they have stomach problems.
- Stress level
Living under a lot of stress, who are in a long-term state of mental tension, depression, anxiety, and fear, are prone to abnormal gastric acid secretion and dysfunction of gastric mucosal vascular constriction, thereby leading to chronic gastric mucosal inflammation causing gastrointestinal dysfunction. Chronic gastric disease is very common these days, it may only take a few years for gastritis to progress to gastric cancer.
Who should have gastroscopy?
You may need a gastroscopy when experiencing:
- Dysphagia (difficulty swallowing)
- Recurrent epigastric pain (discomfort beneath ribcage in upper abdominal region)
- Heartburn
- No Appetite
- Nauseous and Dyspepsy
- Persistent vomiting of unknown cause.
- weight loss
- Gastro-Oesophageal Reflux Disease (GERD)
- Peptic ulcers
- Upper gastrointestinal bleeding (tar-like stool)
- Suspected upper gastrointestinal malignancy
- Cancer screening for high-risk group
If you experience the mentioned symptoms, you should undergo a gastroscopy promptly to ensure timely treatment. The doctor will determine the need for gastroscopy based on the patient's condition.
The gastroscopy is the most reliable method for diagnosing gastric cancer. It allows direct visualization and biopsy of the stomach, making it more accurate for early cancer screening compared to other methods.
Before the gastroscopy, the doctor and anesthesiologist will evaluate the patient's suitability and risks, and obtain informed consent. The pre-operative assessment aims to understand the patient's health status and tolerance to the procedure, in order to plan and minimize the risks of anesthesia and surgery.
What happens during the gastroscopy?
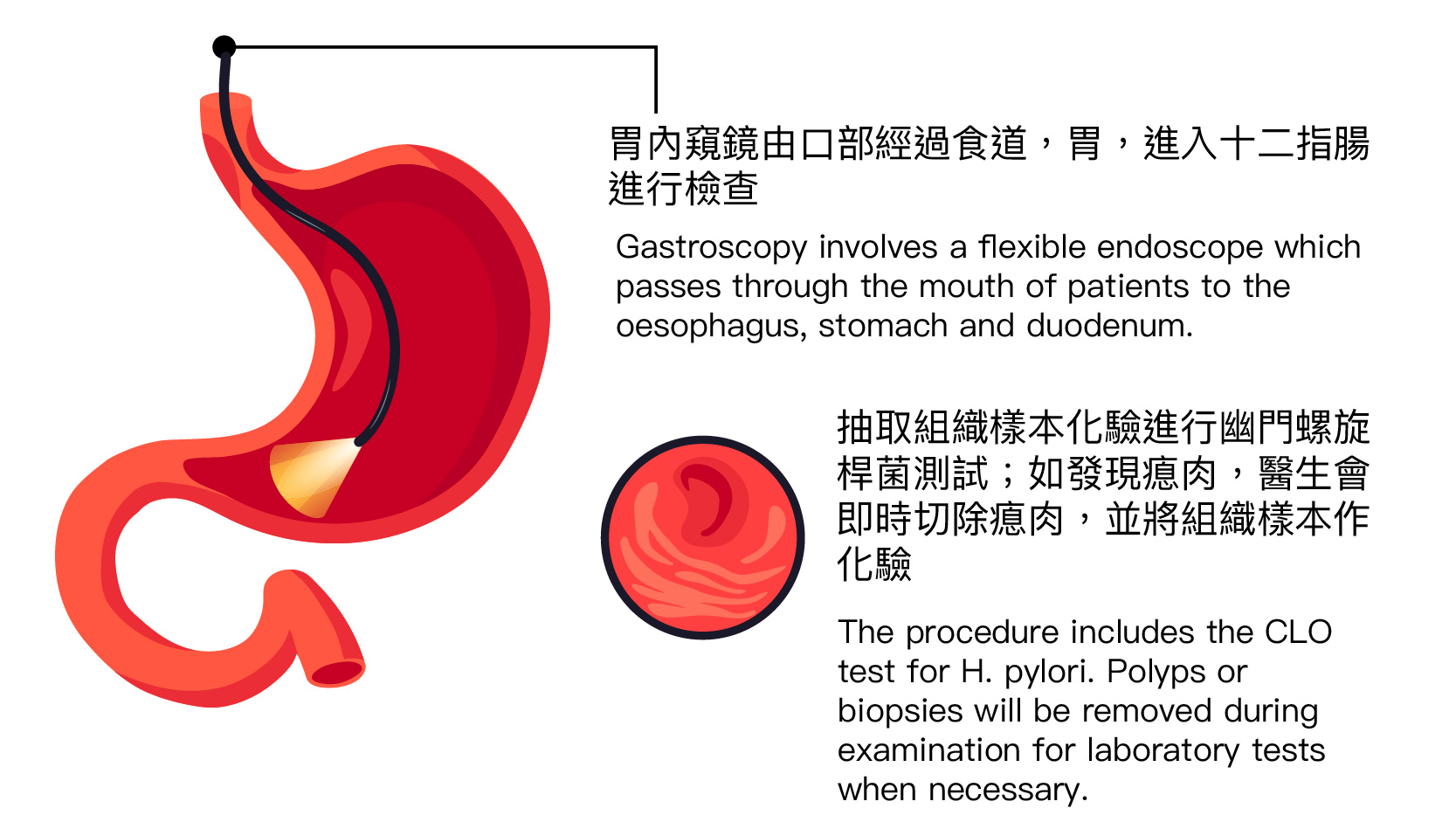
Gastroscopy involves a flexible endoscope which passes through the mouth of patients to the oesophagus, stomach and duodenum to examine if there is any inflammation, stomach polyps, peptic ulcer or tumour diseases. Biopsy will be performed when necessary. The procedure only takes 10 to 15 minutes.
The procedure
 |
 |
 |
 |
|
MAC |
Doctors will insert the gastroscope through the mouth |
Biopsies will be taken for doing H.pylorl testing |
The entire procedure should take around 15 min |
*The method of anaesthesia is determined by doctor according to the individual patient’s condition.
The examination will be performed only when the patient is asleep after monitored anaesthesia care administered by anaesthesiologist, to avoid any discomfort. Anaesthesiologists will participate in providing an anaesthesia opinion prior to the endoscopy. During the procedure, they will constantly monitor the stability of vital signs including pulse, breathing, and blood pressure, making sure vital organs are functioning as normal. Monitored anaesthesia care is a special alternative for patients that require maximum comfort and safety.
The endoscopy will be passing through the mouth of patients to the oesophagus, stomach and duodenum.
A tissue sample will be taken from the stomach lining to diagnose H. pylori infection.
If a suspicious area is seen on the lining of the stomach or oesophagus, the doctor will remove a tissue sample for laboratory test.
How to prepare for the procedure?
- Patients should stop taking antibiotics for six (6) weeks prior to gastroscopy.
- Gastric medications are usually stopped for two (2) weeks prior to gastroscopy.
- Patients need to be fasted for six (6) hours before the procedure.
- Patients are not allowed to drink water and other liquids for two (2) hours prior to the procedure.
- Prior to the procedure, there will be a brief consultation to explain the procedure and the risks involved. A consent form will then be signed by the patient.
- Dentures, accessories and metallic objects will need to be removed for the duration of the procedure.
After the procedure
- The patient will be taken to the recovery room for further monitoring by a team of healthcare professionals. It will take a while for the patient to wake up after the procedure.
- Personal resting suites are provided for patients to take a 15 minutes nap to wear off the sedation. Family members can accompany with the patient for the duration.
- During the gastroscopy, tissue may be removed for laboratory test. As the removal of tissue may cause some small wounds, the patient may feel discomfort for a few days after surgery. Patients are recommended to avoid drinking coffee, milk tea, strong tea, and alcoholic drinks and take postoperative drugs prescribed by the surgeon.
- While the patient is under deep sedation, he/she should be accompanied by at least a friend or a family member aged above 18.
- The sedation and the anaesthetics may temporarily affect one's co-ordination and reasoning skills, driving, drinking alcohol, making any important decision or signing legal document in 24 hours after the procedure should be avoided.
- The effect of local anaesthetics will keep the throat numb for about an hour, during which swallowing is rendered difficult. These should disappear within a day. Please inform your doctor if these symptoms persist.
References
Stomach Cancer. Centre for Health Protection. Available at : https://www.chp.gov.hk/en/healthtopics/content/25/55.html
Anderson WF, et al Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA. 2010;303:1723-1728.
Cancer.gov. Genetics of Gastric Cancer (PDQ®). Available at https://www.cancer.gov/types/stomach/hp/gastric-genetics-pdq#cit/section_1.32
南方周末,拜尔中国公益. 2023打工人胃健康洞察报告. Available at https://irm.infzm.com/2022/pdf/12/Report_on_Stomach_Health_2023.pdf
Săftoiu, A. et al. Role of gastrointestinal endoscopy in the screening of digestive tract cancers in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 2020;52(04):293–304.
Early, D. S. et al. Appropriate use of GI endoscopy. Gastrointestinal Endoscopy 2012;75(6):1127–1131.
American Cancer Society. Signs and Symptoms of Stomach Cancer. Available at : https://www.cancer.org/cancer/types/stomach-cancer/detection-diagnosis-staging/signs-symptoms.html

 3405 8288
3405 8288