Diverticular Disease

Causes and Risk Factors
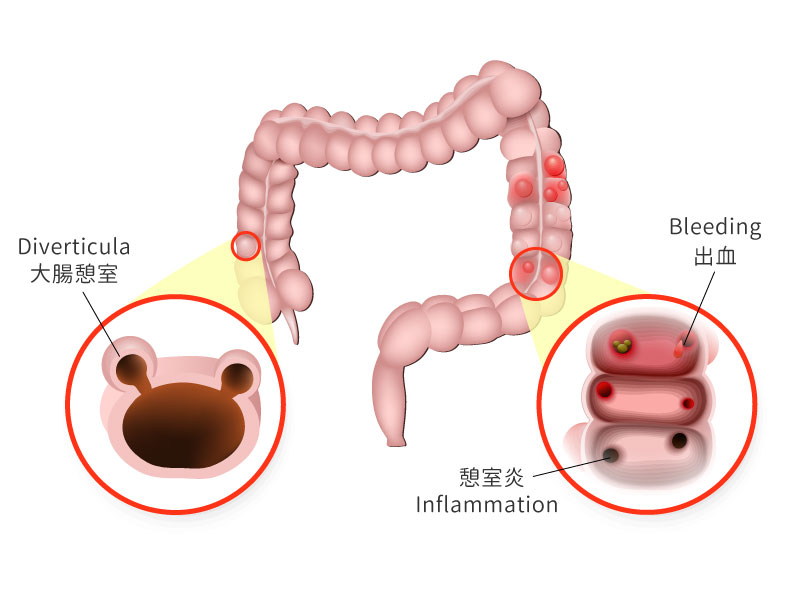
It is possible that the development of colonic diverticula is associated with a low fibre diet. Without fibre to add bulk to the stool, the colon has to work harder than normal to push the stool forward. The pressure from this may cause pouches to form in weak spots along the colon. Diverticula usually develop when naturally weak places in the colon give way under pressure.
The prevalence of diverticula is largely age-dependent, especially after age 40. Besides, people who smoke cigarettes are more likely than non-smokers to experience diverticulitis. Obesity and several drugs are associated with an increased risk of diverticulitis, including steroids, opioids and nonsteroidal anti-inflammatory drugs, such as ibuprofen and naproxen sodium.
What is the difference between diverticulosis and diverticulitis?
Diverticulosis usually cause mild symptoms such as slight abdominal cramps, bloating and constipation. Sometimes, patients may not show symptoms. However, diverticulosis can lead to diverticulitis.
Diverticulitis is inflammation (swelling) and infection in one or more diverticula. Around 10% to 25% of patients with diverticulosis will experience diverticulitis. Diverticulitis happens when there is high pressure in the colon or particles of stool become stuck in these pouches. Therefore, the blood flow is reduced in the colon and infection occurs in the wall of the colon.
Symptoms of diverticular disease and diverticulitis
Potential symptoms of diverticular disease include:
- abdominal pain, usually in the lower part , that tends to come and go and gets worse during or shortly after eating (emptying the bowels eases it)
- constipation, diarrhoea, or both
- occasionally, blood in the stool
If the diverticula become inflamed (diverticulitis), patient may suddenly:
- get constant, more severe abdominal pain
- have a high temperature of 38C or above
- Nausea with decreased appetite, sometimes with vomiting
- get mucus or blood in the stool or rectal bleeding
How Is Diverticulitis Diagnosed?
If you are experiencing the symptoms of diverticulitis, it is important to see your doctor. Doctor will ask questions about your medical history (such as bowel habits, symptoms, diet, and current medications) and perform a physical exam, possibly including an abdominal exam.
To rule out other conditions, one or more diagnostic tests may be ordered. Tests usually include blood tests and CT scanning. For patients with heavy rectal bleeding, the doctor may order a colonoscopy to locate the source of bleeding.
Complications
About 25 percent of diverticulitis cases may develop complications. These complications include:
| Diverticular haemorrhage | Most of the diverticulum haemorrhage occurs in the right colon. The patient may present with blood in stool. There may be a lower chance of turning into a severe haemorrhagic shock. |
| Peritonitis | The mucous membrane is infected or inflamed because of hardened faecal matter retained in the colon, causing abscesses and eventually leading to intestinal perforation and peritonitis. |
| Fistula | Fistula is an abnormal connection that develops between the intestinal tract and the skin. When diverticulitis-related infection spreads outside the colon, the colon's tissue may stick to nearby tissues. It may lead to an infection and further form a fistula. |
| Bowel obstruction | The chronic inflammation can lead to a bowel obstruction, which may cause constipation, thin stools, diarrhoea, bloating, and belly pain. |
Treatment
Mild diverticulitis can be treated with rest, changes in the daily diet and antibiotics. Severe stages of acute, colonic diverticulitis can progress into intestinal perforations with peritonitis. Such cases require surgery.
Prevention
Doing exercise regularly can help with bowel movements and reduce pressure inside colon. Moreover, a high-fibre diet decreases the risk of diverticulitis. Fibre-rich foods, such as fresh fruits and vegetables and whole grains, help the wastes pass more quickly through colon.
*The above information is for reference only, please consult your doctor for detail.
Ref: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3174080/

 3405 8288
3405 8288
